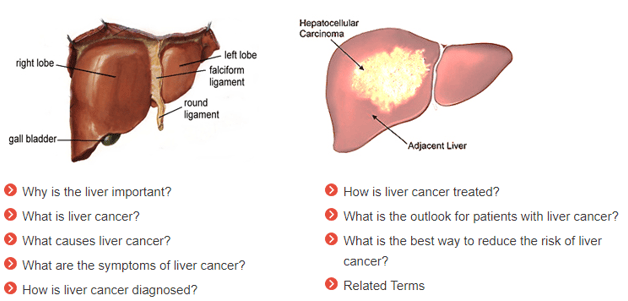
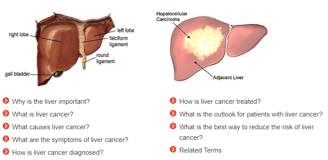
Why is the liver important?
The liver is the second most important organ in your body and is located on the right side. The liver performs many jobs in your body. It processes what you eat and drink into energy and nutrients that it stores for your body to use. The liver also removes harmful substances from your blood.
Liver Cancer
Explore this section to learn more about liver cancer, including a description of the disease and how it's diagnosed.
What is liver cancer?
Liver cancer is the growth and spread of unhealthy cells in the liver. Cancer that starts in the liver is called primary liver cancer. Cancer that spreads to the liver from another organ is called metastatic liver cancer.
What causes liver cancer?
There are several risk factors for liver cancer:
Long-term hepatitis B and hepatitis C infection are linked to liver cancer because they often lead to cirrhosis. Hepatitis B can lead to liver cancer without cirrhosis.
Excessive alcohol use.
Obesity and diabetes are closely associated with a type of liver abnormality called nonalcoholic fatty liver disease (NAFLD) that may increase the risk of liver cancer, especially in those who drink heavily or have viral hepatitis.
Certain inherited metabolic diseases.
Environmental exposure to aflatoxins.
What are the symptoms of liver cancer?
Symptoms may include fatigue, bloating, pain on the right side of the upper abdomen or back and shoulder, nausea, loss of appetite, feelings of fullness, weight loss, weakness, fever, and jaundice (yellowing of the eyes and the skin).
How is liver cancer diagnosed?
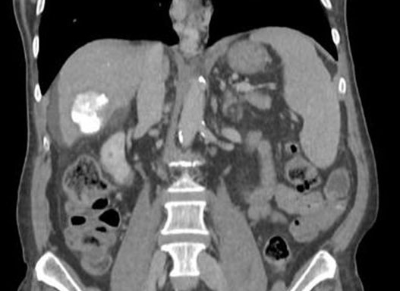
A physical examination or imaging tests may suggest liver cancer. To confirm a diagnosis, blood tests, ultrasound tests, computed tomography (CT) scans, magnetic resonance imaging (MRI), and angiogram needed. Sometimes when picture remains unclear you may also need to get a liver biopsy. During a biopsy, a small piece of liver tissue is removed and studied in the lab.
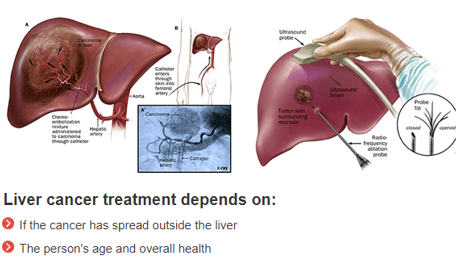
How is liver cancer treated?
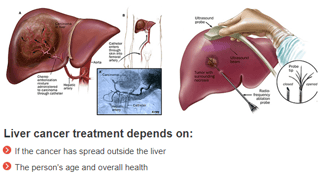
Treatment options if the cancer has not spread and the rest of the liver is healthy are:
Transplant: If the cancer has not spread, for some patients a liver transplant (replacement of the liver) may be an option.
Surgery: If the cancer has been found early and the rest of the liver is healthy, doctors may perform surgery to remove the tumor from the liver (partial hepatectomy).
Radiofrequency/Microwave Ablation: Radiofrequency ablation uses a special probe to destroy cancer cells with heat.
For cancer that has not spread outside the liver:
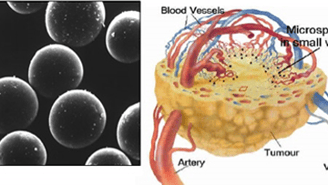
Bland embolization or chemoembolization are procedures in which the blood supply to the tumor is blocked, after giving anticancer drugs (chemoembolization) and one without (bland embolization). Both are given in blood vessels near the tumor.
Internal Radiation therapy (TARE) uses Y-90 particles that emits beta radiation to destroy cancer cells.
For cancer that has spread outside the liver:
Oral medication is available for use in some cases of hepatocellular carcinoma(the most common type of primary liver cancer).
Clinical trials may be an option for some patients.
Talk to your doctor about other options that may be available.
What is the outlook for patients with liver cancer?
A successful liver transplant will effectively cure liver cancer, but it is an option for only a small percentage of patients. Surgical resections are successful in only about one out of three cases. However, scientists are experimenting with several promising new drugs and therapies that could help prolong the lives of people with liver cancer.
What is the best way to reduce the risk of liver cancer?
Steps to reduce the risk of liver cancer include:
Regularly see a doctor who specializes in liver disease
Talk to your doctor about viral hepatitis prevention, including hepatitis A and hepatitis B vaccinations
Take steps to prevent exposure to hepatitis B and hepatitis C.
If you have cirrhosis or chronic liver disease, follow your doctor's recommendations for treatment and be screened regularly for liver cancer
If you are overweight or obese, diabetic, or drink heavily, talk to your doctor
What is it?
A successful liver transplant will effectively cure liver cancer, but it is an option for only a small percentage of patients. Surgical resections are successful in only about one out of three cases. However, scientists are experimenting with several promising new drugs and therapies that could help prolong the lives of people with liver cancer.
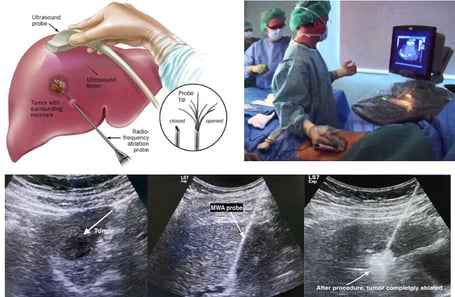
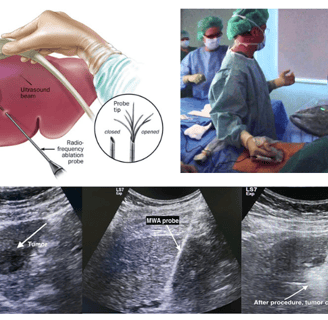
MWA procedure for HCC
Why (Indications)?
Curative treatment for HCC
Considered if transplant/surgery cannot be done
May be combined with RFA for HCC.
Why Not (Contraindication)?
Tumor more than 5 cm in diameter
Extensive tumour infiltration throughout the liver
Large burden of extra-hepatic metastases
What you are to do before procedure (Preparation)?
Visit us in OPD (9-5) with previous lab results (*CBC, LFT, Serum Creatinine, PT/INR), imagingetc.
If you are on blood thinner like Aspirin inform during appointment.
Get admission one day prior to scheduled procedure.
One accompanying person
Need to sign a consent form for procedure
Approx. Stay in hospital?
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 1 Day.
Complications
Mild pain may occur after the procedure.
Resume to work?
You can resume your work after 2-3 days if existing disease allows.
Results: When and How?
After Two or three-month follow-up CT Scan to be done.
For any Queries or Appointment please call +923048267000
Transarterial Chemoembolization (TACE)
What is it?
It is a localized method of administrating chemotherapy directly to the liver tumor via a catheter. One key advantage is the chemotherapy is targeted locally so reducing the systemic side effects of intravenous chemotherapy.
A small puncture is made in blood vessel of thigh region with needle through which wire passed and sheath placed.
Angiography done with catheter under X-ray guidance to look for abnormal region of liver, once we identify the feeding vessels, catheter is placed and blocking agent placed in it.
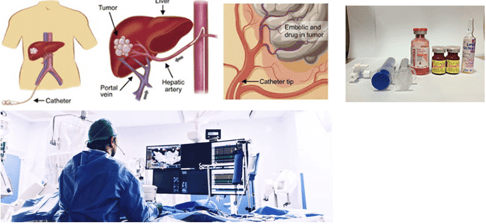

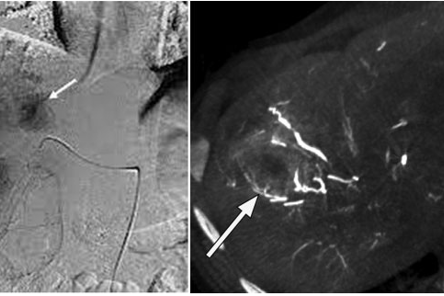


During Procedure (Showing HCC)
Follow up CT after procedure
Why (Indications)?
Most commonly used in the treatment of hepatocellular carcinoma (HCC)
Selective metastatic disease (most commonly from colorectal carcinoma).
As palliative treatment for patient with unresectable HCC or as a bridge to a liver transplant.
Sometimes it is combined with RFA for HCC.
Why Not (Contraindication)?
Absolute contraindications
Extensive tumour infiltration throughout the liver
Large burden of extra-hepatic metastases
Relative contraindications
Portal vein thrombosis
Uncorrectable coagulopathy
What you are to do before procedure (Preparation)?
Visit us in OPD (9-5) with previous lab results (*CBC, LFT, Serum Creatinine, PT/INR), imagingetc.
If you are on blood thinner like Aspirin inform during appointment.
Get admission one day prior to scheduled procedure.
One accompanying person
Need to sign a consent form for procedure
Approx. Stay in hospital?
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 2-3 Days.
Complications
Post embolization syndrome (Pain, nausea, vomiting and low grade fever can last for 7 days).
Resume to work?
You can resume your work after 2-3 days if existing disease allows.
Results: When and How?
After Two or three-month follow-up CT Scan to be done.
For any Queries or Appointment please call +923048267000
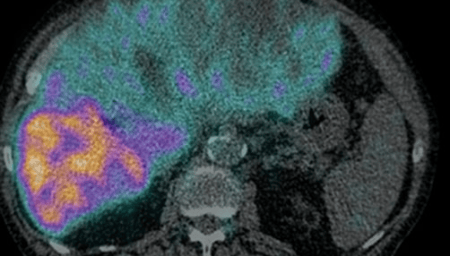
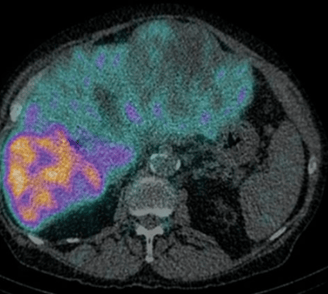
Transarterial Radioembolization (TARE)
What is it?
Radioembolization is a minimally invasive procedure that combines embolization and radiation therapy to treat liver cancer. Tiny glass or resin beads filled with the radioactive isotope yttrium Y-90 are placed inside the blood vessels that feed a tumor. This blocks the supply of blood to the cancer cells and delivers a high dose of radiation to the tumor while sparing normal tissue. It can help extend the lives of patients with inoperable tumors and improve their quality of life.
The radiation from yttrium-90 continually decreases over a two-week period and disappears after 30 days. The tiny microspheres remain in the liver without causing any problems.
It is two step process
STEP 1: Assessment of lung shunt fraction
STEP 2: Radioembolization after 7-10 days
Why Not (Contraindication)?
Severe liver or kidney dysfunction, abnormal blood clotting or a blockage of the bile ducts.
What you are to do before procedure (Preparation)?
Visit us in OPD (9-5) with previous lab results (*CBC, LFT, Serum Creatinine, PT/INR), imagingetc. for proper planning and schedule date. We may require fresh CT angiogram for this.
If you are on blood thinner like Aspirin inform during appointment.
You will receive specific instructions on how to prepare, including any changes that need to be made to your regular medication schedule.
You will be given a sedative during the procedure. You will receive specific instructions on eating and drinking before the procedure and will need to have a relative or friend accompany you and drive you home afterward.
Get admission one day prior to scheduled procedure.
One accompanying person
Need to sign a consent form for procedure
What are the benefits vs. risks?
Benefits
For patients with inoperable tumors, radio-embolization can extend lives from months to years and improve quality of life. In some cases, it may allow for more curative options such as surgery or liver transplantation.
Radioembolization produces fewer side effects compared to standard radiation therapy.
No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
A higher dose of radiation to the tumor is given during radio-embolization than with standard external beam therapy.
Risks
Infection, contrast allergy
Radiation induced lung or bowel injury.
Approx. Stay in hospital?
We have very fast and competent working team (Consultant, fellow, clinical assistant, technician and ward assistant) which provide you comfortable atmosphere and ease your nerves. Usual time of stay is around 2-3 Days.
Complications
Post embolization syndrome (Pain, nausea, vomiting and low grade fever can last for 3 days).
Resume to work?
You can resume your work after 2-3 days if existing disease allows.
Results: When and How?
After Two-month follow-up CT Scan to be done.
For any Queries or Appointment please call +923048267000
Percutaneous Ablation(RFA/MWA)


Have any questions?
If you have any questions about the therapies, feel free to contact us.